Understanding CBT-I: The Key to Beating Insomnia
In this article, you will learn about:
- Ideal weaning time
- Signs that your baby is ready for weaning
- Baby's first solid food
- Correct spoon-feeding technique
- Timing for two meals a day
- Fixing a regular time for solid food feeding
- Baby-led weaning
- Weaning foods to avoid
- Weaning meal ideas
Table of Contents
- What is Cognitive Behavioral Therapy for Insomnia (CBT-I)?
- Effectiveness of Cognitive Behavioral Therapy for Insomnia (CBT-I):
- Advantages of Treating Insomnia with Cognitive Behavioral Therapy (CBT-I):
- Duration of Cognitive Behavioral Therapy for Insomnia (CBT-I):
- Who Is Suitable for Cognitive Behavioral Therapy for Insomnia (CBT-I)?
- After undergoing Cognitive Behavioral Therapy for Insomnia (CBT-I), will I no longer have insomnia?
- Frequently Asked Questions
- Reference
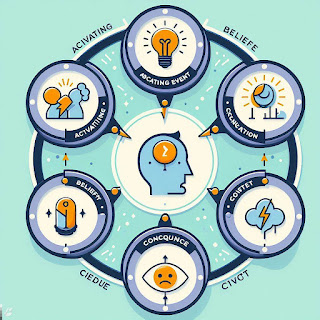
What is Cognitive Behavioral Therapy for Insomnia (CBT-I)?
Cognitive Behavioral Therapy for Insomnia (CBT-I) is a type of psychotherapy that helps people with insomnia change their thoughts and behaviors that interfere with their sleep. Insomnia is a common sleep disorder that makes it hard to fall asleep, stay asleep, or get enough quality sleep. Insomnia can affect your mood, energy, health, and performance.
CBT-I is based on the idea that insomnia is not just a symptom of another problem, but a problem in itself that can be treated. CBT-I helps you identify and modify the negative and unrealistic beliefs that you have about sleep, such as “I can’t function without eight hours of sleep” or “If I don’t sleep well tonight, I will have a terrible day tomorrow”. These beliefs can create anxiety and stress, which make it harder to fall asleep or cause you to wake up during the night.
CBT-I also helps you change your habits and routines that may be keeping you awake, such as going to bed too early or too late, using your bed for activities other than sleep or sex, napping during the day, or spending too much time in bed awake. CBT-I teaches you how to use behavioral strategies, such as stimulus control, sleep restriction, relaxation techniques, and sleep hygiene, to improve your sleep environment, schedule, and quality.
Effectiveness of Cognitive Behavioral Therapy for Insomnia (CBT-I):
CBT-I is currently proven to be the most effective and long-lasting treatment for insomnia based on research. After undergoing CBT-I, 100% of insomnia patients experience improved sleep, with 75% achieving a return to normal sleep. CBT-I can be used either as a standalone treatment or in combination with medication. For individuals with long-term insomnia, choosing medication for rapid sleep improvement should be accompanied by CBT-I to avoid dependency on medication and to provide an opportunity to gradually reduce or discontinue its use.
A meta-analysis of 87 randomized controlled trials involving 11,788 participants found that CBT-I significantly improved sleep onset latency, wake after sleep onset, total sleep time, sleep efficiency, and sleep quality, compared to control groups. These improvements were maintained at follow-up assessments ranging from 3 to 48 months. CBT-I also outperformed medication in terms of long-term efficacy and safety. CBT-I was equally effective for insomnia with or without comorbid conditions, and for different age groups and delivery formats.
A recent study by Harvard Medical School researchers showed that CBT-I can also improve brain function and cognition in individuals with insomnia. The study used functional magnetic resonance imaging (fMRI) to measure brain activity during a working memory task before and after CBT-I or a control intervention. The results showed that CBT-I increased the activation of the dorsolateral prefrontal cortex, a brain region involved in executive functions, such as planning, reasoning, and problem-solving. CBT-I also improved the performance on the working memory task, as well as subjective measures of attention, concentration, and mental fatigue.
Advantages of Treating Insomnia with Cognitive Behavioral Therapy (CBT-I):
| Advantage | Description |
|---|---|
| No physiological or psychological dependency | CBT-I does not lead to dependence on treatment, unlike medication, which can cause tolerance, withdrawal, rebound insomnia, and addiction. |
| No side effects | CBT-I has no adverse effects on health, unlike medication, which can cause daytime sedation, impaired cognition, memory loss, and increased risk of falls, accidents, and mortality. |
| Higher sense of control over sleep | CBT-I empowers individuals to take charge of their sleep by changing their thoughts and behaviors, rather than relying on external factors, such as pills, devices, or substances. |
| Addresses the root cause of chronic insomnia | CBT-I targets the underlying cognitive and behavioral factors that perpetuate insomnia, such as negative beliefs, worry, arousal, and poor sleep habits, rather than masking the symptoms with medication. |
Duration of Cognitive Behavioral Therapy for Insomnia (CBT-I):
Cognitive Behavioral Therapy for Insomnia (CBT-I) is not a quick fix for sleep problems. It requires consistent effort and commitment from the patient to learn and apply new skills and strategies to improve their sleep quality and quantity. Generally, a course of CBT-I lasts about 8-10 weeks, with one session per week and homework assignments between sessions. However, the learning pace and ease of physiological/psychological adjustment vary among individuals. Some patients may need more or less time to achieve their desired sleep goals. Therefore, the duration of CBT-I should be tailored to the patient’s needs and progress, rather than following a rigid schedule.
Who Is Suitable for Cognitive Behavioral Therapy for Insomnia (CBT-I)?
CBT-I is a safe and effective treatment for various types of insomnia, such as difficulty falling asleep, staying asleep, or waking up too early. It is suitable for people who:
- Prefers self-control over sleep without relying on medication. CBT-I helps patients identify and modify the thoughts and behaviors that interfere with their sleep, and teaches them relaxation and coping skills to reduce stress and anxiety related to insomnia.
- Patient enough to gradually improve sleep rather than expecting immediate results. CBT-I does not work overnight. It takes time and practice to change long-standing habits and beliefs that contribute to insomnia. Patients need to be realistic and optimistic about their sleep improvement.
- Open to learning new knowledge and skills, willing to read, practice, and keep records. CBT-I involves active participation from the patient, who needs to follow the therapist’s instructions, complete homework assignments, and monitor their sleep patterns and progress.
- Willing to invest time and money, completing the entire course regularly. CBT-I is not a one-time intervention. It requires regular attendance and adherence to the treatment plan. CBT-I may also incur some costs, depending on the availability and coverage of health insurance.
- Simple insomnia issues (evaluation by a psychologist to determine the need for other treatment plans). CBT-I is designed to treat primary insomnia, which is insomnia that is not caused by another medical or psychiatric condition. If the insomnia is secondary to another disorder, such as depression, anxiety, chronic pain, or sleep apnea, CBT-I may not be sufficient or appropriate. In such cases, the underlying disorder needs to be treated first or concurrently with CBT-I.
CBT-I is suitable for short-term/long-term insomnia, medication/non-medication users, especially for long-term insomnia sufferers. CBT-I has been shown to be more effective than medication in the long run, as it addresses the root causes of insomnia and prevents relapse. CBT-I can also help patients who want to reduce or stop their use of sleeping pills, as it can reduce the dependence and tolerance that may develop with chronic use of medication.
After undergoing Cognitive Behavioral Therapy for Insomnia (CBT-I), will I no longer have insomnia?
During the treatment process, most patients experience gradual improvement in sleep. However, not all patients achieve complete freedom from insomnia within 8-10 weeks. Typically, after the treatment ends, patients need to continue using the learned techniques for self-therapy until the insomnia problem disappears. Since insomnia is not resolved overnight, it is unrealistic to expect immediate relief. Sufficient time is needed to practice new techniques, establish new habits, and adjust physiological and psychological responses.
CBT-I cannot prevent brief episodes of insomnia from reoccurring in the future. In fact, when facing significant life stress, insomnia is a normal and inevitable response. Usually, when stress is relieved, or when we adapt to stress, insomnia disappears. After undergoing CBT-I, individuals no longer fear insomnia and can immediately use the acquired knowledge and techniques for self-adjustment when brief insomnia episodes occur, preventing them from worsening into chronic insomnia.
According to a recent meta-analysis of 87 studies, CBT-I has been found to have lasting effects on sleep outcomes, with sustained improvements up to 12 months after treatment. Another study found that CBT-I can also improve daytime functioning, mood, and quality of life in patients with insomnia. Therefore, CBT-I is not only a treatment for insomnia, but also a way to enhance overall well-being.
Frequently Asked Questions
What are the common side effects of CBT-I?
CBT-I is generally well-tolerated and safe for most patients. However, some patients may experience some mild and temporary side effects during the initial stages of treatment, such as:
| Side effect | Explanation | Remedy |
|---|---|---|
| Increased sleepiness | CBT-I may involve restricting the time spent in bed to increase sleep efficiency and consolidate sleep. This may lead to some sleep deprivation and increased sleepiness during the day. | This side effect is expected and will subside as the sleep quality improves. Patients should avoid napping during the day, as this may interfere with the sleep consolidation process. Patients should also avoid driving or operating heavy machinery if they feel too sleepy. |
| Increased anxiety | CBT-I may involve challenging and changing the negative thoughts and beliefs that cause anxiety and worry about sleep. This may temporarily increase the anxiety level as the patients confront their fears and doubts. | This side effect is normal and will decrease as the patients learn to cope with their anxiety and develop more positive and realistic attitudes towards sleep. Patients should practice relaxation techniques, such as deep breathing, progressive muscle relaxation, or mindfulness, to reduce their anxiety and calm their mind. |
| Increased frustration | CBT-I may involve setting and following a regular sleep schedule, which may require some changes in the patients’ lifestyle and habits. This may cause some frustration and resistance, especially if the patients do not see immediate results or face some setbacks. | This side effect is understandable and will diminish as the patients see the benefits of CBT-I and gain more confidence and control over their sleep. Patients should be patient and persistent, and focus on the long-term goals rather than the short-term difficulties. Patients should also seek support and feedback from their therapist, family, or friends, to help them cope with the frustration and stay motivated. |
These side effects are not serious and do not outweigh the benefits of CBT-I. However, if the side effects persist or worsen, patients should consult their therapist and discuss possible adjustments or alternatives to the treatment plan.
Can I use CBT-I with medication?
CBT-I can be used with or without medication, depending on your preference and situation. Some people may choose to use medication as a short-term or occasional aid to help them fall asleep or cope with acute insomnia. However, medication is not a long-term solution for insomnia, as it may have side effects, lose effectiveness, or cause dependence or withdrawal symptoms. Therefore, if you are taking medication for insomnia, you should discuss with your doctor and therapist the possibility of tapering or discontinuing it gradually, while undergoing CBT-I. CBT-I can help you reduce or eliminate your need for medication, by addressing the root causes of your insomnia and teaching you natural and effective ways to improve your sleep.
However, some people may need to continue taking medication for other reasons, such as a coexisting medical or mental health condition that affects their sleep. In this case, you should consult with your doctor and therapist about the best way to combine CBT-I with medication, and how to monitor and manage any potential interactions or complications. CBT-I can still help you enhance your sleep quality and quantity, by complementing the effects of medication and helping you cope with any residual or rebound insomnia. CBT-I can also help you prevent or reduce the negative impact of insomnia on your physical and mental health.
Reference
- Mitchell, M. D., Gehrman, P., Perlis, M., & Umscheid, C. A. (2012). Comparative effectiveness of cognitive behavioral therapy for insomnia: a systematic review. BMC family practice, 13, 40. https://doi.org/10.1186/1471-2296-13-40
- Morin, C. M., & Benca, R. (2012). Chronic insomnia. The Lancet, 379(9821), 1129-1141. https://doi.org/10.1016/S0140-6736(11)60750-2
- Qaseem, A., Kansagara, D., Forciea, M. A., Cooke, M., & Denberg, T. D. (2016). Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Annals of internal medicine
You may be interested in these articles:
Genetics of Sleep Disorders: Unveiling the Mystery
Unlocking the Secrets: What is Cognitive Behavioral Therapy for Insomnia (CBT-I)? Explained
Why Is It Easier to Fall Asleep on the Couch as You Get Older?




Comments
Post a Comment